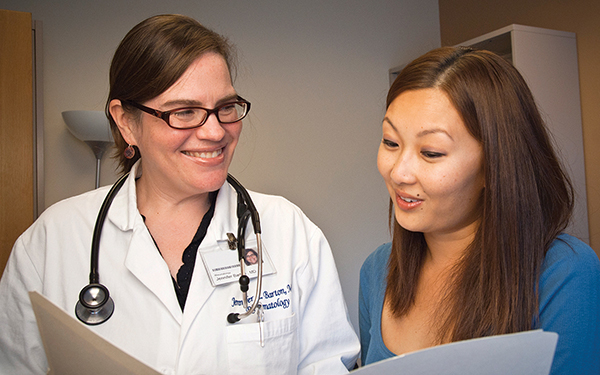
Tool update and digitization to facilitate shared decision-making in rheumatoid arthritis (RA Decision Aid 2.0)
Grant info: Gerlinger Award, (PI:Barton)
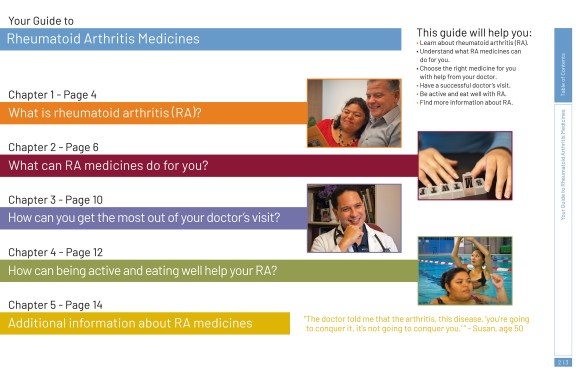
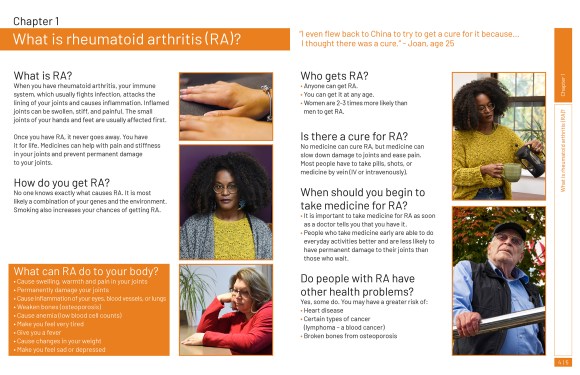
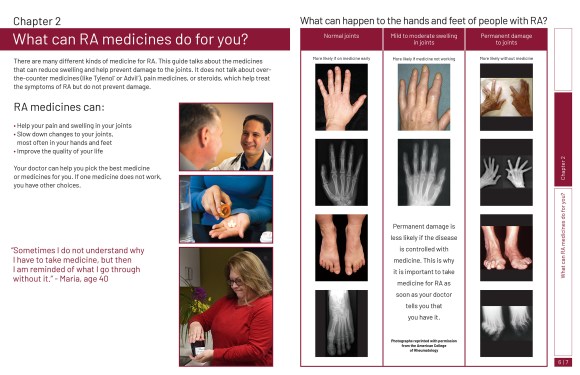
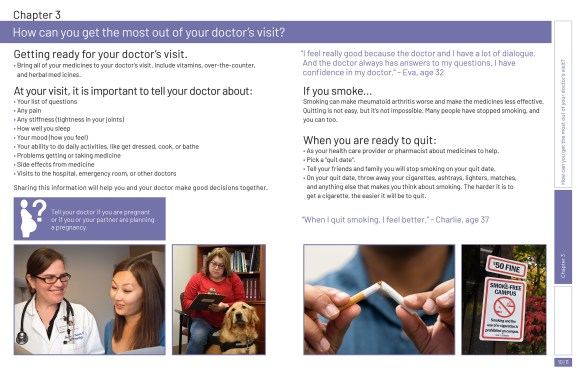
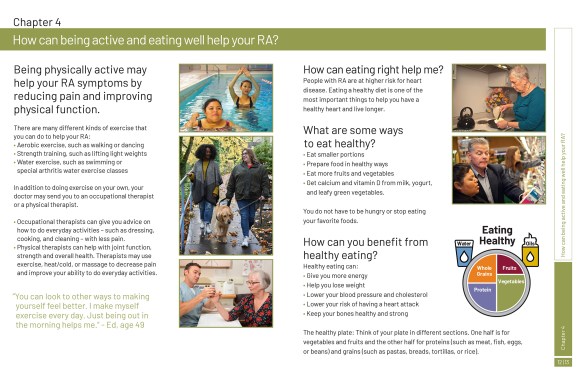
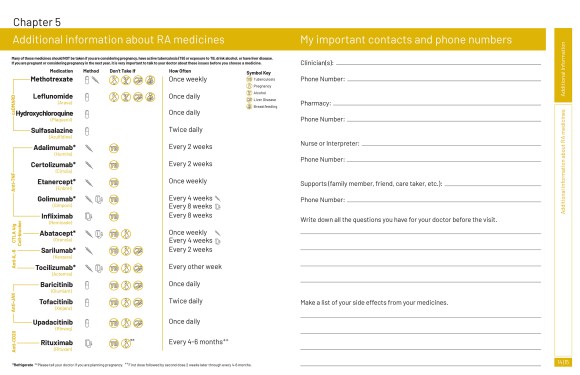
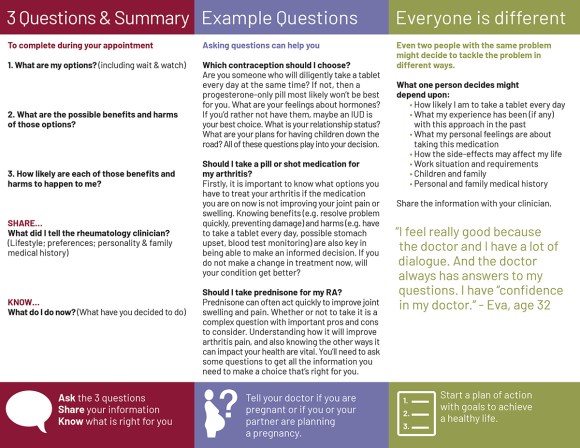
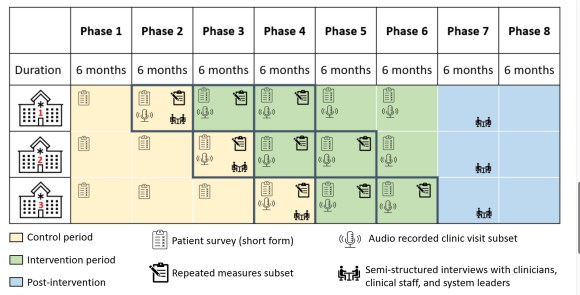
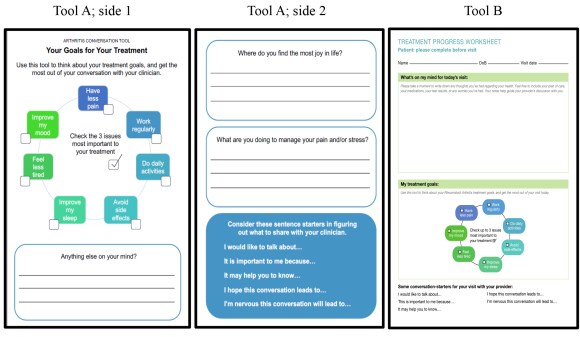
RA Decision Aid 2.0 is low literacy, multilingual medication summary guide, and decision aid tool for RA patients and clinicians developed by a multi-stakeholder team including Dr. Barton. This tool was designed to facilitate shared decision-making when patients and clinicians collaborate to identify how to best address the patient’s situation. Past research has shown the tool improves patient knowledge and decision quality, but it has not been tested broadly. To keep pace with recent therapeutic advances and most effectively support shared decision-making for all RA patients, RA Decision Aid 2.0 aimed to update and digitize the RA medication summary guide and decision aid; and to evaluate the acceptability and feasibility of the use of the updated, print, and digital medication summary guide and RA Decision Aid 2.0 among persons with RA and their clinicians. This project updated and revised tools in order to be more widely disseminated to rheumatology clinics, clinicians, and RA patients within the VA system and beyond to increase the quality and efficacy of care; thus meeting the VA goal of contributing to national research which improves healthcare. In addition, a major objective of this project was to increase patient involvement in care.